Recognizing the importance of readmission metrics to all those involved in the healthcare industry, HCUP has collected data from the Nationwide Readmissions Data from 2009 to the present day and categorized it for better parsing. One of the purposes of the examination of this data is to gauge the performance of the aforementioned measures of the HHRP and PfP in reducing readmissions rates.
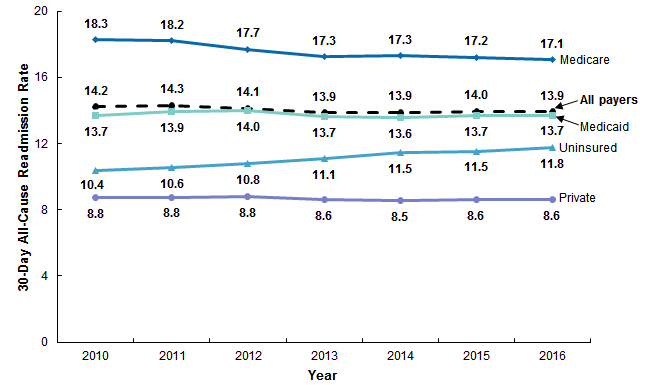
The most recent HCUP Statistical Brief presented statistics on 30-day all-cause readmissions among patients aged 1 year and up. The four different types of payers were, in order from highest rate of readmission to lowest, those on Medicare, then Medicaid, the uninsured, and those with private insurance. The trends for each were as follows: Medicare trended downward from 18.3 to 17.1 %, Medicaid held very constant just above an average of 13.7%, the uninsured’s rates increased from 10.4 to 11.8%, and those with private insurance stayed steady around 8.8%.