The below information is sourced from the U.S. Food and Drug Administration’s “SARS-CoV-2 Viral Mutations: Impact on COVID-19 Tests:”
Genetic Variations: Background and Considerations
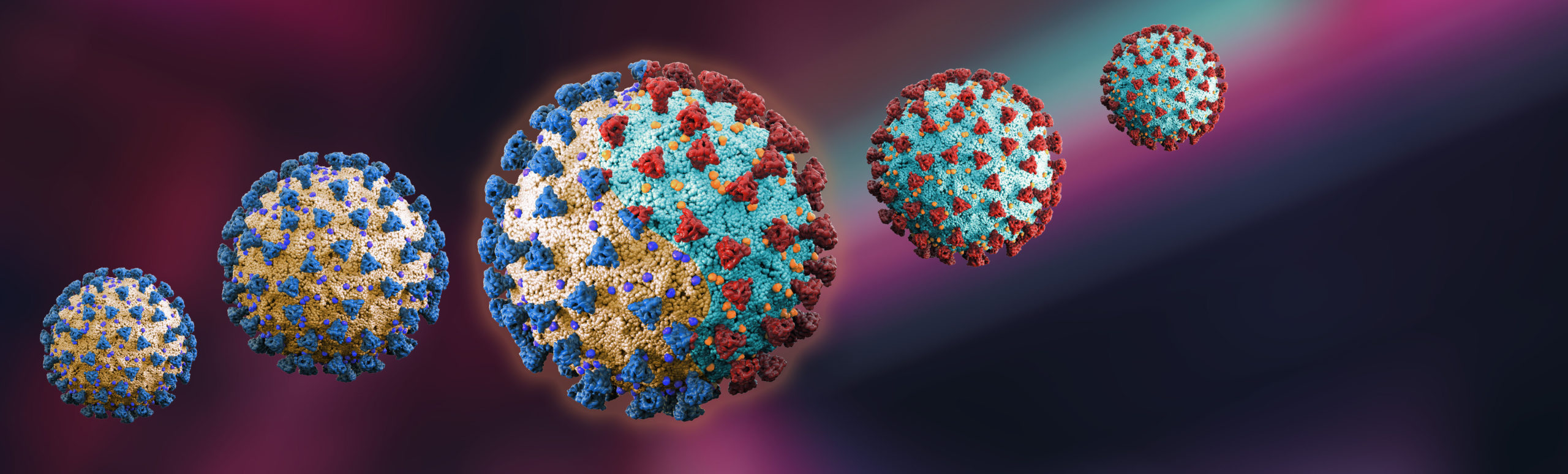
The SARS-CoV-2 virus has mutated over time, resulting in genetic variation in the population of circulating viral strains over the course of the COVID-19 pandemic. Molecular, antigen, and serology tests are affected by viral mutations differently due to the inherent design differences of each test.
This page provides information regarding the impact of viral mutations on COVID-19 tests, recommendations for clinical laboratory staff and health care providers, and information about certain tests for which the FDA has identified potential impacts on performance due to SARS-CoV-2 genetic mutations. The FDA will update this page as significant new information becomes available.
A mutation (viral mutation or genetic mutation) of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) virus is a change in the genetic sequence of the SARS0-CoV-2 virus when compared with a reference sequence such as Wuhan-Hu1 (the first genetic sequence identified) or USA-WA1/2020 (the first identified in the United States). A new variant (virus variant or genetic variant) of SARS-CoV-2 may have one or more mutations that differentiate it from the reference sequence or predominant virus variants already circulating in the population. Variants of SARS-CoV-2 can have different characteristics. For example, some may spread more easily or show signs of resistance to existing treatment options and some may have no impact when compared with previous and currently circulating virus.
The presence of mutations in the SARS-CoV-2 virus in a patient sample can potentially impact test performance. The impact of mutations on a test’s performance is influenced by several factors, including the sequence of the variant, the design of the test, and the prevalence of the variant in the population.
The FDA has collaborated with stakeholders to better understand the public health impact of new SARS-CoV-2 variants and their impact on test performance, has been routinely monitoring publicly available databases, and has coordinated efforts to evaluate the impact of new virus variants on tests that have received Emergency Use Authorization (EUA).
In February 2021, the FDA issued the Policy for evaluating Impact of Mutations on COVID-19 Tests to provide a policy and recommendations on evaluating the potential impact of emerging and future viral mutations of SARS-CoV-2 on COVID-19 tests for the duration of the COVID-19 public health emergency, including considerations for test designs to minimize the impact of viral mutations and recommendations for ongoing monitoring.
General Information for Clinical Laboratory Staff and Healthcare Providers
Clinical laboratory staff and health care providers should be aware that false negative results may occur with any molecular test for the detection of SARS-CoV-2 if a mutation occurs in the part of the virus’ genome assessed by that test. The FDA first alerted clinical laboratory staff and health care providers of this issue through a January 8, 2021 safety alert: https://www.fda.gov/medical-devices/letters-health-care-providers/genetic-variants-sars-cov-2-may-lead-false-negative-results-molecular-tests-detection-sars-cov-2.
Changes in the viral genome can result in changes to viral proteins and, therefore, can also impact the performance of an antigen or serology test.
The FDA recommends clinical laboratory staff and health care providers who use SARS-CoV-2 tests:
- Be aware that genetic variants of SARS-CoV-2 arise regularly, and false negative test results can occur.
- Be aware that molecular tests that use multiple genetic targets to determine a final result are less likely to be impacted by increased prevalence of genetic variants.
- Consider negative results in combination with clinical observations, patient, history, and epidemiological information.
- Consider repeat testing with a different EUA authorized or FDA cleared molecular diagnostic test (with different genetic targets) if COVID-19 is still suspected after receiving a negative test result.
In addition to these general recommendations, the FDA is providing recommendations for the use of specific tests impacted by genetic variation. For further information on these test recommendations, please read their full article linked above.
Stay well, stay informed, and stay tuned!
